Haldol
23 June, 2023
Heparin
23 June, 2023Haloperidol
Generic name:
Haloperidol
Drug class:
Typical antipsychotic (butyrophenone class), first-generation antipsychotic
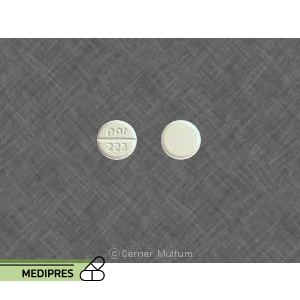
Dosage form:
- Tablets
- Oral solution
- Injectable solution (intramuscular and intravenous)
- Decanoate long-acting injectable
Root of administration:
- Oral
- Intramuscular (IM)
- Intravenous (IV)
Dose:
- Oral: Typically 0.5 mg to 5 mg two to three times daily; maintenance doses range from 1 mg to 20 mg per day depending on indication and patient response
- IM: 2 to 10 mg per dose, repeated every 4 to 8 hours as needed; maximum dosage varies by severity
- IV: Used with caution, dosing similar to IM but requires careful monitoring
- Decanoate IM (long acting): Initial loading dose usually 10 to 20 times the oral daily dose, given every 4 weeks
- Dose adjustments needed based on clinical response, age, hepatic/renal function
Mechanism of action:
Haloperidol primarily acts as a potent antagonist of dopamine D2 receptors in the central nervous system, reducing dopaminergic neurotransmission. This effect alleviates psychotic symptoms by dampening dopamine activity in the mesolimbic pathway. It also has some antagonistic effects on alpha-1 adrenergic receptors and other receptors, contributing to its side effect profile.
Drug usage cases:
- Schizophrenia and other psychotic disorders
- Acute psychosis and delirium
- Manic episodes in bipolar disorder
- Tourette’s syndrome and other tic disorders
- Severe behavioral problems in children (off-label)
- Nausea and vomiting refractory to other treatments (off-label)
- Agitation and severe anxiety states (off-label use in emergency settings)
Drug contra indications:
- Hypersensitivity to haloperidol or any component of the formulation
- Parkinson’s disease or other dopamine-depleting conditions
- Severe central nervous system depression or coma
- Severe cardiac conditions including prolonged QT interval, known arrhythmias
- Use in patients with dementia-related psychosis (risk of increased mortality)
- Use in neonates or premature infants for avoidance of neuroleptic malignant syndrome (for injectable forms specifically)
Side effects:
- Extrapyramidal symptoms (EPS): dystonia, parkinsonism, akathisia, tardive dyskinesia
- Neuroleptic malignant syndrome (rare but potentially fatal)
- Sedation and drowsiness
- Orthostatic hypotension
- Dry mouth
- Constipation
- Weight gain (less common than atypical antipsychotics)
- Elevated prolactin levels leading to gynecomastia, galactorrhea, menstrual disturbances
- QT prolongation and cardiac arrhythmias
- Blurred vision
- Urinary retention
- Leukopenia, neutropenia, and agranulocytosis (rare)
- Seizures (may lower seizure threshold)
- Hyperthermia
- Elevated liver enzymes
- Injection site reactions (for IM/long-acting formulations)
Warnings:
- Monitor for extrapyramidal symptoms and treat accordingly
- Risk of neuroleptic malignant syndrome—discontinue immediately if suspected
- Monitor cardiac function due to QT prolongation risk, particularly in patients with cardiac disease or on other QT-prolonging drugs
- Use cautiously in elderly patients, especially those with dementia (increased mortality risk)
- Orthostatic hypotension risk; advise patients to rise slowly from sitting or lying positions
- Avoid abrupt discontinuation to prevent withdrawal symptoms and relapse
- Regular monitoring of blood counts recommended due to rare hematological adverse reactions
- May impair judgment and ability to perform tasks requiring alertness
- Use caution in patients with epilepsy or history of seizures
- Potential for hyperprolactinemia and related hormonal effects
- Injection route: risk of local pain, swelling, and rarely abscess formation; long-acting formulations require careful dosing and monitoring
Use during pregnancy or breastfeeding:
Haloperidol is classified as FDA Pregnancy Category C. Animal studies have shown adverse effects on the fetus, but there are no well-controlled studies in pregnant women. Use during pregnancy is only recommended if the potential benefit justifies the potential risk to the fetus.
Potential risks include extrapyramidal symptoms and withdrawal symptoms in neonates exposed in the third trimester. Caution is advised, especially near delivery.
Haloperidol is excreted in breast milk in small amounts. Nursing mothers should be monitored for possible adverse effects in the infant, such as sedation or extrapyramidal symptoms. Breastfeeding is generally not recommended during treatment unless the benefits outweigh the risks.